When the Dentist’s Chair Triggers the Brain: What EEG Reveals About Kids and Dental Anxiety

New research shows that dental visits aren't just uncomfortable for some kids—they can be neurologically overwhelming.
For many children, a trip to the dentist is a minor inconvenience. For others, it’s a sensory overload that triggers a cascade of neurological stress. Now, thanks to an innovative study using electroencephalography (EEG), we have a clearer picture of what actually happens inside a child’s brain during dental procedures—and why traditional care may not be enough for those with special needs.
This study, conducted by a team of researchers in Gujarat, monitored brain activity in children during routine dental care. What they discovered wasn’t just important—it may change the way pediatric dentistry approaches neurodivergent children.
The Study: Listening to the Brain in Real Time
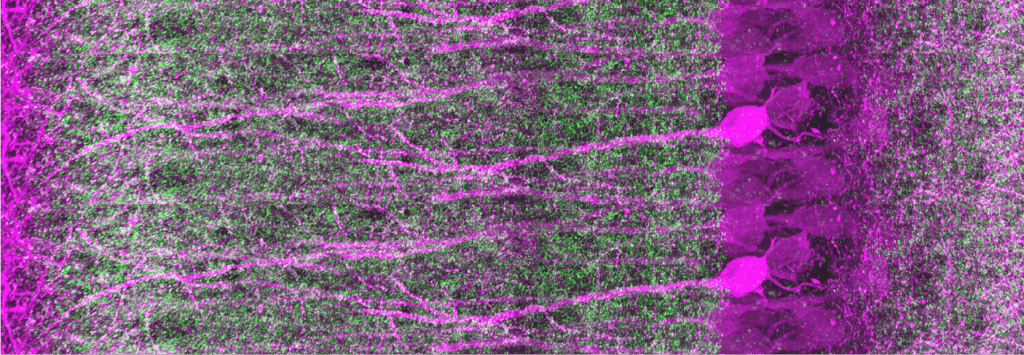
The researchers recruited 16 children aged 6 to 12, split into two groups: neurotypical and neurodivergent (children diagnosed with conditions such as autism, ADHD, and sensory processing disorders). All underwent simple, non-invasive dental procedures like fluoride treatment and scaling—while wearing a custom-fitted, 24-channel EEG cap that tracked their brain activity throughout the experience.
Each child went through three stages:
- Resting baseline
- During the dental procedure
- Post-procedure relaxation
EEG recordings captured how each child’s brain reacted at every step—revealing a fascinating and sometimes concerning picture.
What the Brainwaves Revealed
The key differences between the two groups became clear almost immediately:
- Neurotypical children showed an initial spike in brain activity, followed by adaptation and calming as the procedure progressed.
- Neurodivergent children, on the other hand, showed sustained high levels of stress-related activity throughout the procedure—especially in beta and gamma wave bands, associated with anxiety, attention, and sensory processing.
Statistically significant findings included:
- Elevated frontal theta and beta activity in neurodivergent children (p < 0.01), signaling heightened tension.
- Persistent stress markers, like frontal alpha asymmetry, remained even after the procedures were completed.
- Increased mu rhythm suppression, a marker of tactile hypersensitivity, especially in children with sensory impairments.
One Size Does Not Fit All
Perhaps the most telling discovery was this: while 64% of neurotypical children adapted during the treatment, only 43% of children with special needs showed any meaningful adaptation—despite the use of calming techniques like music and tactile interaction.
Procedures like scaling (a common dental cleaning method) caused significant spikes in beta activity in neurodivergent participants. Meanwhile, the variation in EEG responses was 42% higher in the special needs group—suggesting that standard protocols don’t work uniformly, even within that group.
These neurological findings mirrored the behavioral challenges dentists often face: reluctance, resistance, distress, or even panic.
Why This Matters
It’s easy to assume that dental fear is just emotional. But EEG scans tell another story: for some children, dental care triggers a neurological stress loop that’s hard to break.
This matters because:
- Long-term avoidance of dental care can lead to serious oral health issues, infections, and chronic pain.
- Repeated traumatic experiences in the dental chair can result in lifelong dental phobia.
- Sensory overload during treatment can negatively affect a child’s behavior, communication, and emotional well-being far beyond the clinic walls.
In short: ignoring these neurological responses doesn’t just make dental visits harder—it risks the child’s long-term health.
Toward a More Inclusive Dental Future
This study offers a roadmap for transforming pediatric dental care into a more empathetic, neuro-aware experience. Recommendations include:
- Tailoring procedures to individual needs, based on sensory profiles or neurological markers.
- Using calming interventions like tactile stimulation, controlled audio environments, and visual distraction tools.
- Allowing longer adaptation times and flexible scheduling.
- Training dental professionals in neurodiversity-sensitive protocols.
Most importantly, it reinforces that behavior is not the full story—brain activity reveals stress even when a child appears calm or compliant.
Final Thoughts: Listening to What the Brain Is Saying
We often ask children to “be brave” or “sit still” in the dentist’s chair. But what if their brains are screaming behind the silence?
Thanks to EEG technology, we can now begin to see what was invisible before—and start making changes that don’t just clean teeth, but protect mental health, respect neurodiversity, and foster trust in medical care.